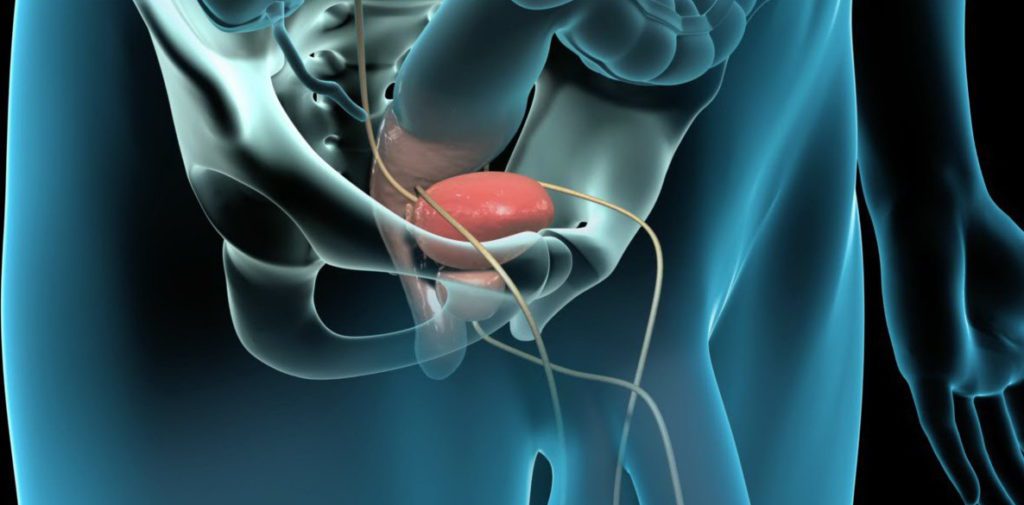
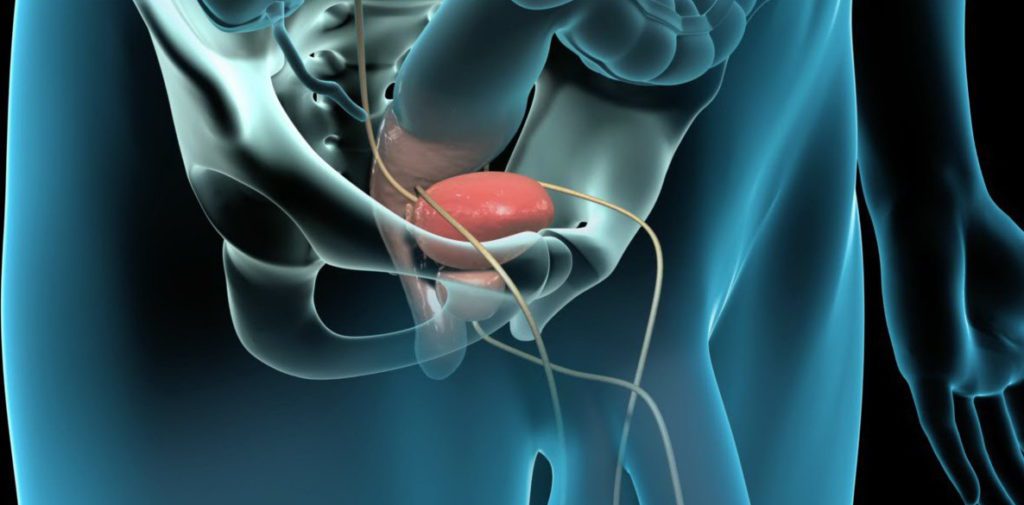
Prostatitis is inflammation of the prostate gland, the walnut-sized gland located below a man’s bladder. The prostate gland secretes fluid that, along with sperm, forms semen.
There are different types of prostatitis, one of which is chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). This is the most common type. Young and middle-aged men are more likely to develop CP/CPPS, but it can happen at any age.
CP/CPPS may be classified as inflammatory or non-inflammatory.
In inflammatory cases, urine, semen, and fluid secreted by the prostate contain infection-fighting cells. But these fluids don’t contain bacteria.
When CP/CPPS is non-inflammatory, no infection-fighting cells and no bacteria are found in the fluid.
Men with CP/CPPS can experience chronic discomfort or pain in the groin, genitals, perineum (the area between the anus and the genitals), or bladder. They may have pain with urination and ejaculation as well. Many feel anxious about the situation.
But symptoms don’t happen to every man with CP/CPPS. Also, symptoms may come and go on their own.
CP/CPPS can be hard to diagnose because its symptoms are similar to other medical conditions, like kidney and bladder problems. Also, some researchers believe that CP/CPPS is not related to the prostate gland but may be caused by pelvic floor muscle strain instead.
Men usually undergo a digital rectal exam, during which their doctor inserts a lubricated, gloved finger into the rectum. By doing this, the doctor can feel any abnormalities in the prostate gland.
Doctors may also analyze urine and prostatic fluid. In some cases, blood tests, ultrasounds, MRIs, or biopsies are ordered to rule out other conditions.
CP/CPPS can also be difficult to treat and, unfortunately, it cannot always be cured. It can also take some time to find what best relieves a man’s symptoms. Some strategies for treating CP/CPPS symptoms include the following:
Medications.
Anti-inflammatory, pain medications, and muscle relaxants may be recommended. Alpha-blockers, which help relax muscles around the prostate, may also help. Some doctors prescribe antibiotics for CP/CPPS, but this treatment option is controversial.
Heat.
Some men find relief by taking a hot bath or by applying a heating pad or hot water bottle to the affected area.
Changes in diet.
Spicy foods and caffeinated or acidic drinks can aggravate symptoms for some men.
Lifestyle changes.
Activities that make symptoms worse, like bicycle riding, may need to be avoided.
Pillows.
Experimenting with different pillows or cushions may help a man who is uncomfortable while seated.
Prostatic massages.
These massages can help release some pressure around the prostate.
Counseling.
Psychological issues among men with CP/CPPS are common. Men with the condition have considerably higher levels of anxiety than those without it. Some experts believe that psychological problems are part of the cause of CP/CPPS. Such problems could also develop as a result. In either case, talking to a counselor may help men cope with this aspect of CP/CPPS.
Men with severe CP/CPPS may require surgery.
Sometimes, CP/CPPS gets better on its own.
Most men with CP/CPPS can have sex as they did before. However, it may be uncomfortable at times, especially during a pain flare-up. Couples may need to take a break from sex until the discomfort passes.