Male Infertility
Male Infertility

Definition
Up to 15 percent of couples are infertile. This means they aren't able to conceive a child even though they've had frequent, unprotected sexual intercourse for a year or longer. In up to half of these couples, male infertility plays a role.
Male infertility is due to low sperm production, abnormal sperm function or blockages that prevent the delivery of sperm. Illnesses, injuries, chronic health problems, lifestyle choices and other factors can play a role in causing male infertility.
Not being able to conceive a child can be stressful and frustrating, but a number of male infertility treatments are available.
Symptoms
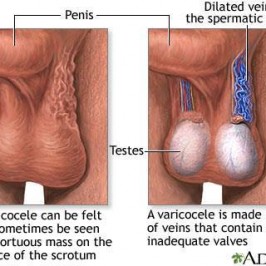
The main sign of male infertility is the inability to conceive a child. There may be no other obvious signs or symptoms. In some cases, however, an underlying problem such as an inherited disorder, hormonal imbalance, dilated veins around the testicle, or a condition that blocks the passage of sperm causes signs and symptoms.
Although most men with male infertility do not notice symptoms other than inability to conceive a child, signs and symptoms associated with male infertility include:
- Problems with sexual function — for example, difficulty with ejaculation or small volumes of fluid ejaculated, reduced sexual desire or difficulty maintaining an erection (erectile dysfunction)
- Pain, swelling or a lump in the testicle area
- Recurrent respiratory infections
- Inability to smell
- Abnormal breast growth (gynecomastia)
- Decreased facial or body hair or other signs of a chromosomal or hormonal abnormality
- Having a lower than normal sperm count (fewer than 15 million sperm per milliliter of semen or a total sperm count of less than 39 million per ejaculate)
When to see a doctor
See a doctor if you have been unable to conceive a child after a year of regular, unprotected intercourse or sooner if you have any of the following:
- Have erection or ejaculation problems, low sex drive, or other problems with sexual function
- Have pain, discomfort, a lump or swelling in the testicle area
- Have a history of testicle, prostate or sexual problems
- Have had groin, testicle, penis or scrotum surgery
Causes
Male fertility is a complex process. To get your partner pregnant, the following must occur:
- You must produce healthy sperm.Initially, this involves the growth and formation of the male reproductive organs during puberty. At least one of your testicles must be functioning correctly, and your body must produce testosterone and other hormones to trigger and maintain sperm production.
- Sperm have to be carried into the semen.Once sperm are produced in the testicles, delicate tubes transport them until they mix with semen and are ejaculated out of the penis.
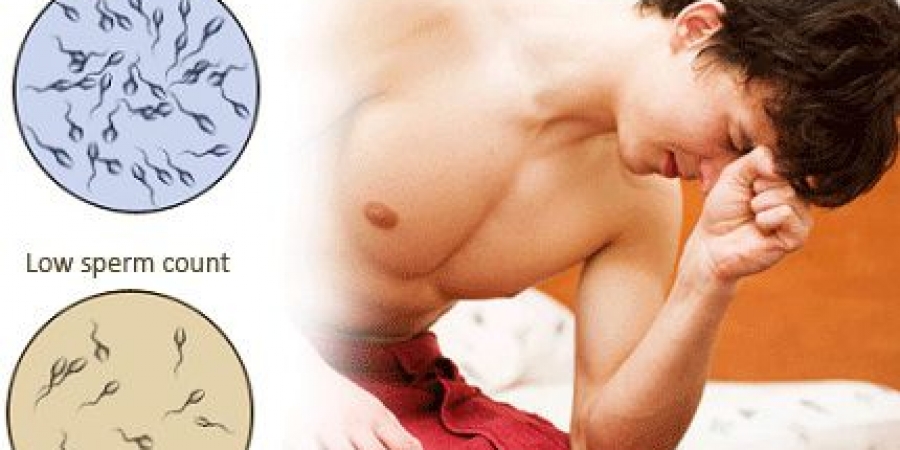
- There needs to be enough sperm in the semen.If the number of sperm in your semen (sperm count) is low, it decreases the odds that one of your sperm will fertilize your partner's egg. A low sperm count is fewer than 15 million sperm per milliliter of semen or fewer than 39 million per ejaculate.
- Sperm must be functional and able to move.If the movement (motility) or function of your sperm is abnormal, the sperm may not be able to reach or penetrate your partner's egg.
Medical causes
Problems with male fertility can be caused by a number of health issues and medical treatments. Some of these include:
- A varicocele is a swelling of the veins that drain the testicle. It's the most common reversible cause of male infertility. Although the exact reason that varicoceles cause infertility is unknown, it may be related to abnormal testicular temperature regulation. Varicoceles result in reduced quality of the sperm.
Treating the varicocele can improve sperm numbers and function, and may potentially improve outcomes when using assisted reproductive techniques such as in vitro fertilization.
- Some infections can interfere with sperm production or sperm health or can cause scarring that blocks the passage of sperm. These include inflammation of the epididymis (epididymitis) or testicles (orchitis) and some sexually transmitted infections, including gonorrhea or HIV. Although some infections can result in permanent testicular damage, most often sperm can still be retrieved.
- Ejaculation issues.Retrograde ejaculation occurs when semen enters the bladder during orgasm instead of emerging out the tip of the penis. Various health conditions can cause retrograde ejaculation, including diabetes, spinal injuries, medications, and surgery of the bladder, prostate or urethra.
Some men with spinal cord injuries or certain diseases can't ejaculate semen, even though they still produce sperm. Often in these cases sperm can still be retrieved for use in assisted reproductive techniques.
- Antibodies that attack sperm.Anti-sperm antibodies are immune system cells that mistakenly identify sperm as harmful invaders and attempt to eliminate them.
- Cancers and nonmalignant tumors can affect the male reproductive organs directly, through the glands that release hormones related to reproduction, such as the pituitary gland, or through unknown causes. In some cases, surgery, radiation or chemotherapy to treat tumors can affect male fertility.
- Undescended testicles.In some males, during fetal development one or both testicles fail to descend from the abdomen into the sac that normally contains the testicles (scrotum). Decreased fertility is more likely in men who have had this condition.
- Hormone imbalances.Infertility can result from disorders of the testicles themselves or an abnormality affecting other hormonal systems including the hypothalamus, pituitary, thyroid and adrenal glands. Low testosterone (male hypogonadism) and other hormonal problems have a number of possible underlying causes.
- Defects of tubules that transport sperm.Many different tubes carry sperm. They can be blocked due to various causes, including inadvertent injury from surgery, prior infections, trauma or abnormal development, such as with cystic fibrosis or similar inherited conditions.
Blockage can occur at any level, including within the testicle, in the tubes that drain the testicle, in the epididymis, in the vas deferens, near the ejaculatory ducts or in the urethra.
- Chromosome defects.Inherited disorders such as Klinefelter's syndrome — in which a male is born with two X chromosomes and one Y chromosome (instead of one X and one Y) — cause abnormal development of the male reproductive organs. Other genetic syndromes associated with infertility include cystic fibrosis, Kallmann's syndrome and Kartagener's syndrome.
- Problems with sexual intercourse.These can include trouble keeping or maintaining an erection sufficient for sex (erectile dysfunction), premature ejaculation, painful intercourse, anatomical abnormalities such as having a urethral opening beneath the penis (hypospadias), or psychological or relationship problems that interfere with sex.
- Celiac disease.A digestive disorder caused by sensitivity to gluten, celiac disease can cause male infertility. Fertility may improve after adopting a gluten-free diet.
- Certain medications.Testosterone replacement therapy, long-term anabolic steroid use, cancer medications (chemotherapy), certain antifungal medications, some ulcer drugs and certain other medications can impair sperm production and decrease male fertility.
- Prior surgeries.Certain surgeries may prevent you from having sperm in your ejaculate, including vasectomy, inguinal hernia repairs, scrotal or testicular surgeries, prostate surgeries, and large abdominal surgeries performed for testicular and rectal cancers, among others. In most cases, surgery can be performed to either reverse these blockage or to retrieve sperm directly from the epididymis and testicles.
Environmental causes
Overexposure to certain environmental elements such as heat, toxins and chemicals can reduce sperm production or sperm function. Specific causes include:
- Industrial chemicals.Extended exposure to benzenes, toluene, xylene, pesticides, herbicides, organic solvents, painting materials and lead may contribute to low sperm counts.
- Heavy metal exposure.Exposure to lead or other heavy metals also may cause infertility.
- Radiation or X-rays.Exposure to radiation can reduce sperm production, though it will often eventually return to normal. With high doses of radiation, sperm production can be permanently reduced.
- Overheating the testicles.Elevated temperatures impair sperm production and function. Although studies are limited and are inconclusive, frequent use of saunas or hot tubs may temporarily impair your sperm count.
Sitting for long periods, wearing tight clothing or working on a laptop computer for long stretches of time also may increase the temperature in your scrotum and may slightly reduce sperm production.
Health, lifestyle and other causes
Some other causes of male infertility include:
- Illicit drug use.Anabolic steroids taken to stimulate muscle strength and growth can cause the testicles to shrink and sperm production to decrease. Use of cocaine or marijuana may temporarily reduce the number and quality of your sperm as well.
- Alcohol use.Drinking alcohol can lower testosterone levels, cause erectile dysfunction and decrease sperm production. Liver disease caused by excessive drinking also may lead to fertility problems.
- Tobacco smoking.Men who smoke may have a lower sperm count than do those who don't smoke. Secondhand smoke also may affect male fertility.
- Emotional stress.Stress can interfere with certain hormones needed to produce sperm. Severe or prolonged emotional stress, including problems with fertility, can affect your sperm count.
- Obesity can impair fertility in several ways, including directly impacting sperm themselves as well as by causing hormone changes that reduce male fertility.
Certain occupations including welding or those involving prolonged sitting, such as truck driving, may be associated with a risk of infertility. However, the research to support these links is mixed.
Risk factors
Risk factors linked to male infertility include:
- Smoking tobacco
- Using alcohol
- Using certain illicit drugs
- Being overweight
- Having certain past or present infections
- Being exposed to toxins
- Overheating the testicles
- Having experienced trauma to the testicles
- Having a prior vasectomy or major abdominal or pelvic surgery
- Having a history of undescended testicles
- Being born with a fertility disorder or having a blood relative with a fertility disorder
- Having certain medical conditions, including tumors and chronic illnesses, such as sickle cell disease
- Taking certain medications or undergoing medical treatments, such as surgery or radiation used for treating cancer
Tests and diagnosis
Many infertile couples have more than one cause of infertility, so it's likely you will both need to see a doctor. It might take a number of tests to determine the cause of infertility. In some cases, a cause is never identified.
Infertility tests can be expensive and might not be covered by insurance — find out what your medical plan covers ahead of time.
Diagnosing male infertility problems usually involves:
- General physical examination and medical history.This includes examining your genitals and asking questions about any inherited conditions, chronic health problems, illnesses, injuries or surgeries that could affect fertility. Your doctor might also ask about your sexual habits and about your sexual development during puberty.
- Semen analysis.You can provide a semen sample by masturbating and ejaculating into a special container at the doctor's office or by using a special condom to collect semen during intercourse.
Your semen is then sent to a laboratory to measure the number of sperm present and look for any abnormalities in the shape (morphology) and movement (motility) of the sperm. The lab will also check your semen for signs of problems such as infections.
Often sperm counts fluctuate significantly from one specimen to the next. In most cases, several semen analysis tests are done over a period of time to ensure accurate results. If your sperm analysis is normal, your doctor will likely recommend thorough testing of your female partner before conducting any more male infertility tests.

Your doctor might recommend additional tests to help identify the cause of your infertility. These can include:
- Scrotal ultrasound.This test uses high-frequency sound waves to produce images inside your body. A scrotal ultrasound can help your doctor see if there is a varicocele or other problems in the testicles and supporting structures.
- Hormone testing.Hormones produced by the pituitary gland, hypothalamus and testicles play a key role in sexual development and sperm production. Abnormalities in other hormonal or organ systems might also contribute to infertility. A blood test measures the level of testosterone and other hormones.
- Post-ejaculation urinalysis.Sperm in your urine can indicate your sperm are traveling backward into the bladder instead of out your penis during ejaculation (retrograde ejaculation).
- Genetic tests.When sperm concentration is extremely low, there could be a genetic cause. A blood test can reveal whether there are subtle changes in the Y chromosome — signs of a genetic abnormality. Genetic testing might be ordered to diagnose various congenital or inherited syndromes.
- Testicular biopsy.This test involves removing samples from the testicle with a needle. If the results of the testicular biopsy show that sperm production is normal your problem is likely caused by a blockage or another problem with sperm transport.
However, this test is not commonly used to diagnose the cause of infertility.
- Specialized sperm function tests.A number of tests can be used to check how well your sperm survive after ejaculation, how well they can penetrate an egg, and whether there's any problem attaching to the egg. Generally, these tests are rarely performed and often do not significantly change recommendations for treatment.
- Transrectal ultrasound.A small, lubricated wand is inserted into your rectum. It allows your doctor to check your prostate, and look for blockages of the tubes that carry semen (ejaculatory ducts and seminal vesicles).
Treatments and drugs
Often, an exact cause of infertility can't be identified. Even if an exact cause isn't clear, your doctor might be able to recommend treatments or procedures that will result in conception.
In cases of infertility, the female partner is also recommended to be checked. This can help to determine if she will require any specific treatments or if proceeding with assisted reproductive techniques is appropriate.
Treatments for male infertility include:
- For example, a varicocele can often be surgically corrected or an obstructed vas deferens repaired. Prior vasectomies can be reversed. In cases where no sperm are present in the ejaculate, sperm can often be retrieved directly from the testicles or epididymis using sperm retrieval techniques.
- Treating infections.Antibiotic treatment might cure an infection of the reproductive tract, but doesn't always restore fertility.
- Treatments for sexual intercourse problems.Medication or counseling can help improve fertility in conditions such as erectile dysfunction or premature ejaculation.
- Hormone treatments and medications.Your doctor might recommend hormone replacement or medications in cases where infertility is caused by high or low levels of certain hormones or problems with the way the body uses hormones.
- Assisted reproductive technology (ART).ART treatments involve obtaining sperm through normal ejaculation, surgical extraction or from donor individuals, depending on your specific case and wishes. The sperm are then inserted into the female genital tract, or used to perform in vitro fertilization or intracytoplasmic sperm injection.