Sperm harvesting is entirely different from a diagnostic testicular biopsy since in this setting the goal is not to identify what is happening in the testis but instead it is to find sperm. Only men with no sperm in their ejaculate (azoospermia) need to have sperm retrieved directly from the testis or epididymis.
This may involve a simple aspiration for men who have a blockage or require much more extensive sampling of the testis for men who have a sperm production problem. As a result, there is a significant difference in the amount of time it takes, the need for anesthesia and the equipment utilized.
Very few tests allow for an accurate prediction of whether or not sperm will be found in the testes of men with testicular problems. Genetic testing may give insight into the chance of finding sperm but are not absolute. The pattern of the problem of the testis found at the time of a diagnostic testicular biopsy may be slightly predictive but again there is no finding that absolutely predicts the presence or absence of sperm. Other blood tests including hormonal studies are not predictive.
Finally, even having sperm found on previous harvesting session does not guarantee that sperm will be found on future harvesting attempts. Thus, diagnostic testicular biopsy is not routinely performed in patients who are to undergo testicular harvesting of sperm when the cause of their zero sperm count is already established through other means.
The Timing of Sperm Retrieval
The timing of sperm harvesting in conjunction with the IVF cycle is a difficult matter to resolve. There are advantages for and against doing the sperm harvesting prior to the IVF cycle or in conjunction with the harvesting of the female partner’s eggs. The ultimate decision is made by the preference of the IVF program. Performing the harvesting in advance and freezing the sperm until the eggs are harvested allows the couple to make an informed decision whether to go forward with IVF since in most circumstances the chance of finding sperm may be only 60% or less.
Moreover, it is difficult for many couples to undergo operative procedures the same day since it requires their enlisting other resources to help them get to and from the hospital and assistance at home. IVF laboratories frequently prefer to work with fresh rather than frozen sperm and thus their desire to have fresh sperm trumps any other consideration.
As a result, simple sperm retrievals are typically performed the day of egg retrieval. Simple sperm retrievals are procedures performed in men with known obstruction who make sperm without a problem. These procedures are summarized below, and include Testicular Sperm Aspiration (TESA), Percutaneous Sperm Aspiration (PESA), and Testicular Sperm Extraction (TESE).
Microdissection TESE is a much more involved procedure and is performed the day before the female partner’s egg retrieval. Microdissection TESE is carefully coordinated with the reproductive endocrinologist and is performed at designated times on a quarterly basis.
Which Sperm Retrieval Procedure is Recommended?
There are numerous ways to harvest sperm from a man with normal sperm production and a blockage. The simplest and most cost-effective is an aspiration of sperm. This is routinely performed under local anesthesia and takes approximately ten minutes.
Harvesting sperm from a man with a testicular problem is much more difficult and often takes several hours. The ideal procedure, Microdissection Testicular Sperm Extraction, is performed with the aid of a surgical microscope whereby the chances of finding sperm are increased and the amount of tissue taken out of the testis can be minimized.
It is important to understand that the microscope utilized in the operating room does not have sufficient magnification to see sperm but instead just helps sort out which tubules within the testis are more likely to contain sperm. Small amounts of tissue are sent to the IVF laboratory during the course of the procedure so that they can assess whether sufficient numbers of sperm have been harvested. A more powerful microscope is used by the IVF laboratory to evaluate this tissue. Repeated biopsies from one or both testes are obtained until sufficient sperm has been harvested for that IVF cycle. Extra sperm may be harvested to preserve for future cycles of IVF in case the current cycle is unsuccessful or the couple desires more children in the future. This procedure can take as long as four hours depending upon how quickly sperm are found.
Here is a summary of the procedures available for sperm harvesting:
Testicular sperm aspiration (TESA)
Testicular sperm aspiration (TESA) is a procedure performed for men who are having sperm retrieved for in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI). It is done with local anesthesia in the operating room or office and is coordinated with their female partner’s egg retrieval. A needle is inserted in the testicle and tissue/sperm are aspirated. TESA is performed for men with obstructive azoospermia (s/p vasectomy). Occasionally, TESA doesn’t provide enough tissue/sperm and an open testis biopsy is needed.
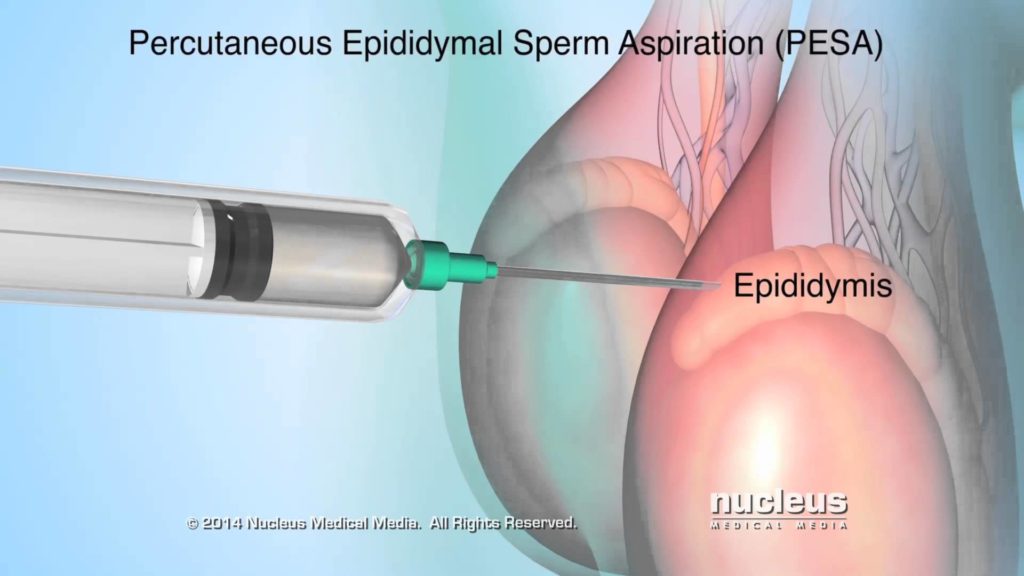
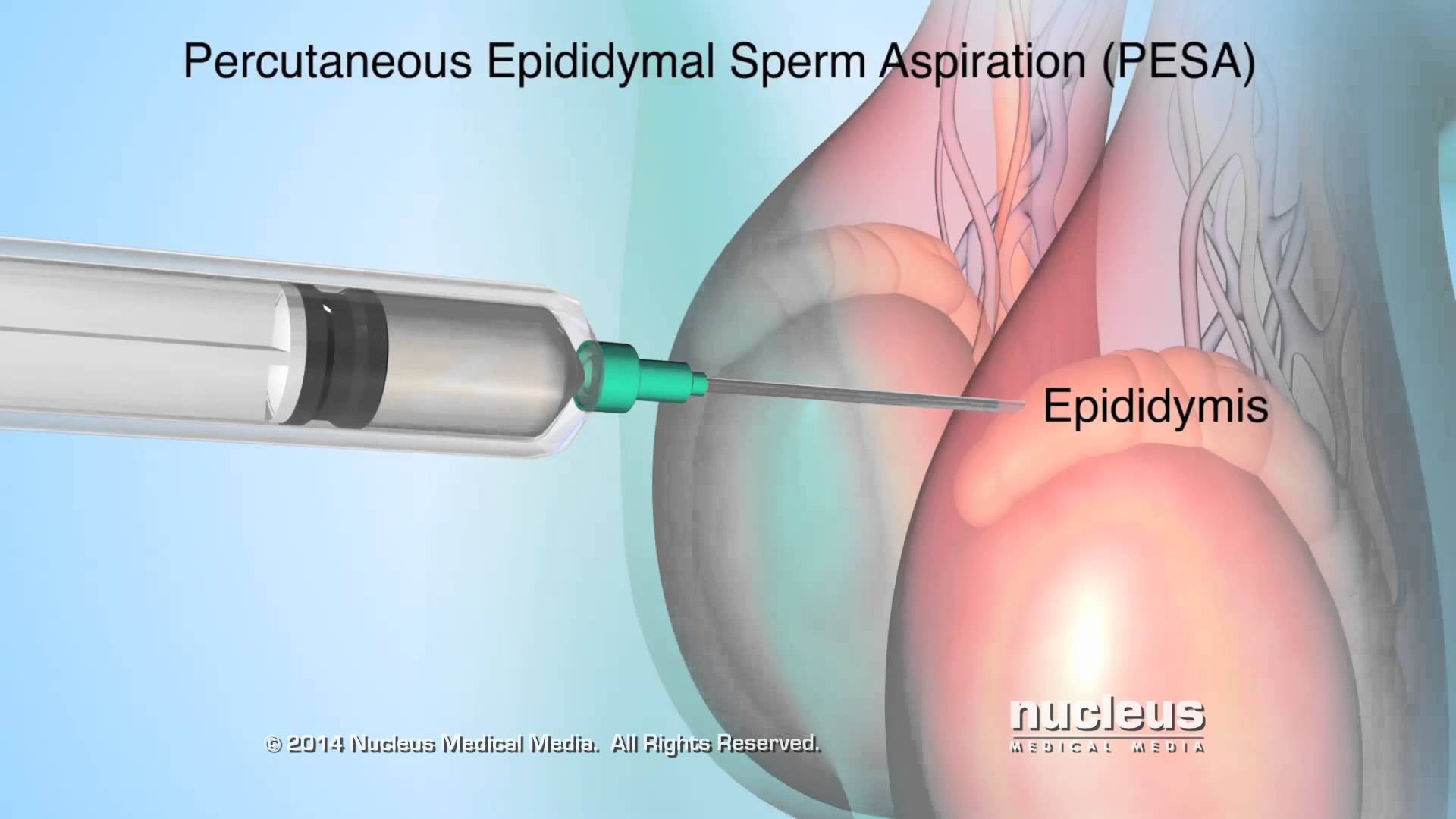
Percutaneous Epididymal Sperm Aspiration (PESA)
PESA is a procedure performed for men who are having sperm retrieved for in vitro fertilization/intracytoplasmic sperm injection (IVF/ICSI) who have obstructive azoospermia from either a prior vasectomy or infection. It is done with local anesthesia in the operating room or office and is coordinated with their female partner’s egg retrieval.
Testicular sperm extraction (TESE)
TESE involves making a small incision in the testis and examining the tubules for the presence of sperm. It is either done as a scheduled procedure or is coordinated with their female partner’s egg retrieval. TESE is usually performed in the operating room with sedation, but can be performed in the office with local anesthesia alone. Patients usually cryopreserve sperm during this procedure for future IVF/ICSI. Microdissection TESE has replaced this as the optimal form of retrieval for men with no sperm in their ejaculate (azoospemia) from a problem with production.
Microepididymal Sperm Aspiration (MESA)
MESA is a procedure performed for men who have vasal or epididymal obstruction (s/p vasectomy, congenital bilateral absence of the vas deferens). It is either done as a scheduled procedure or is coordinated with their female partner’s egg retrieval. MESA is performed in the operating room with general anesthesia utilizing the operating microscope. Patients usually cryopreserve sperm during this procedure for future IVF/ICSI. MESA allows for an extensive collection of sperm as compared to aspiration techniques, and is the preferred method of retrieval for men with congenital bilateral absence of the vas deferens (CBAVD).
Microdissection TESE (microdissection testicular sperm extraction)
Microdissection TESE is a procedure performed for men who have a sperm production problem and are azoospermic. Microdissection TESE is performed in the operating room with general anesthesia under the operating microscope. Micro TESE is carefully coordinated with the female partner’s egg retrieval, and is performed the day before egg retrieval. This allows for each partner to be there for the other’s procedure. Patients frequently have donor sperm backup in the case that sperm are not found in the male partner. Micro TESE has significantly improved sperm retrieval rates in azoospermic men, and is a safer procedure since less testicular tissue is removed. Patients cryopreserve sperm during this procedure for future IVF/ICSI.