There are many things men can do to improve erectile function. Many of them provide other health benefits as well, so it makes sense to give them a try.
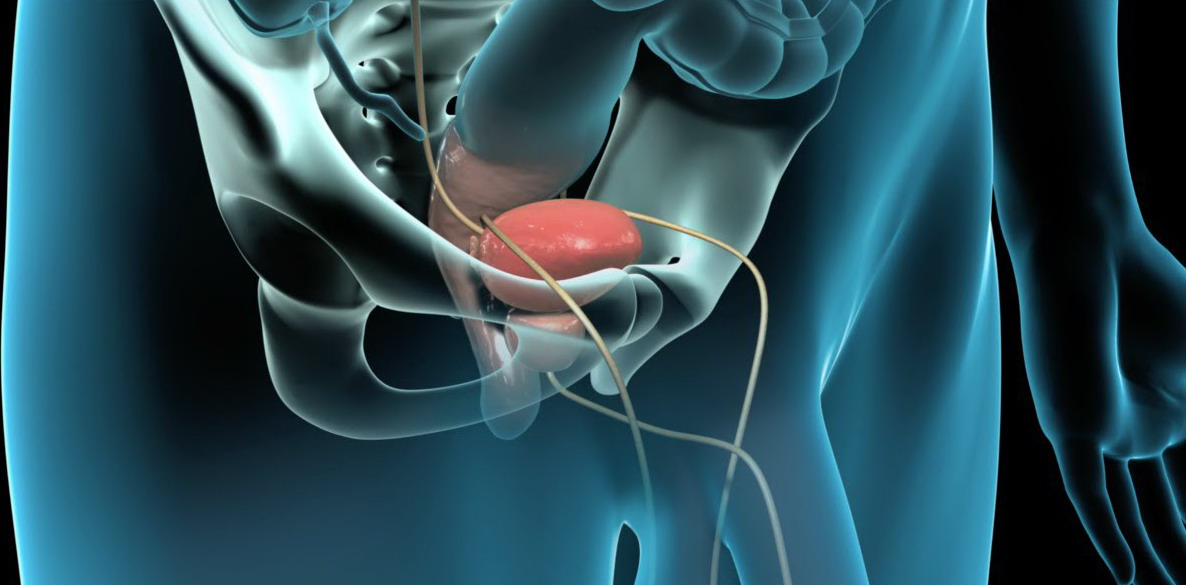
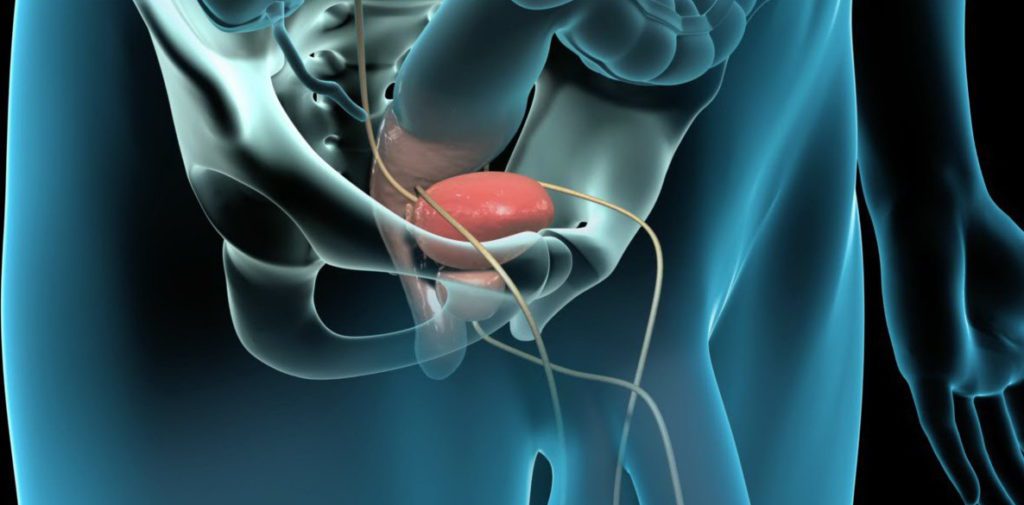
Before considering these lifestyle changes, it’s helpful to remember the role of penile blood flow in forming and maintaining an erection.
When a man is sexually stimulated, penile arteries widen and smooth muscle tissue relaxes. As a result, the penis fills with blood, which gives the erection its firmness.
Often, erectile dysfunction occurs when there are problems with blood flow. Many of these suggestions improve blood flow, but there are other factors, like nerve damage, that can be involved.
Exercise
Many men find that their erectile function improves when they exercise regularly. Exercise helps to keep blood flowing smoothly, including blood to the penis. Research has shown that men who are more physically active are at a lower risk of developing erectile dysfunction.
Men should consult their doctors before beginning a regular exercise program to ensure that the type of exercise they choose is appropriate for them.
Maintain a healthy weight
Obesity can damage blood vessels that allow blood into the penis for an erection. Studies have shown that heavier men tend to have more erectile problems, which may improve after the men lose weight.
Weight loss may also help erectile function by decreasing inflammation, increasing testosterone, alleviating depression, and boosting confidence.
Don’t smoke (or quit if you do smoke)
Scientific studies have found that men who smoke are more likely to develop erectile dysfunction than nonsmoking men. This likelihood appears to increase with the amount of cigarettes smoked over time. Men who stop smoking often see an improvement in their erectile function.
Eat a healthy diet
Research has shown that eating a Mediterranean diet may improve erectile function for some men. This diet includes fruits, vegetables, grains, and olive oil. Research has also shown that men without erectile dysfunction were more likely to eat lots of fruits, vegetables, nuts, and fish, and whole grains.
Control blood sugar and manage diabetes
Many men with diabetes have erectile problems. High blood sugar can damage blood vessels, nerves, and erectile tissue.
Blood vessels may be more susceptible to atherosclerosis – hardening of the arteries – in diabetic men. This means that plaques build up in the arteries, making it more difficult for blood to flow freely into the penis and form an erection.
Nerve damage, or neuropathy, can cause signaling problems between the brain and the penis. A man’s brain may register sexual stimulation, but if the “message” doesn’t reach the penis, there will be erectile problems.
High blood sugar can also interfere with the production of chemicals needed for an erection, like the neurotransmitter nitric oxide.
Other chemicals associated with diabetes can stiffen erectile tissue, leading to valve problems and “venous leak.” When this happens, the erection cannot be maintained because blood leaks out of the penis and back into the body.
Manage blood pressure
High blood pressure, or hypertension, is a common cause of erectile dysfunction, as it can interfere with penile blood flow.
While it’s important to manage high blood pressure, medications for this condition may also affect erectile function. It appears that older drugs, such as diuretics and beta-blockers, are more likely to have sexual side effects than newer ones. A man’s physician can help him decide on the best treatment options.
Manage depression
Depression is associated with erectile dysfunction, although it is unclear whether one directly causes the other. A man’s depression may lead to erectile difficulties. However, erectile dysfunction may also make him depressed.
Nevertheless, managing depression may help alleviate erectile dysfunction. It is important to note, however, that some commonly prescribed medications for depression, such as selective serotonin-reuptake inhibitors (SSRIs), have sexual side effects. A man may need to try different medications, with a physician’s guidance, to determine which one works best for him.
Remain sexually active
In a Finnish study of men between the ages of 55 and 75, men who had intercourse less than once a week were twice as likely to have erectile dysfunction than those who had intercourse once a week. The researchers concluded that regular intercourse protects against erectile dysfunction.
Be careful when bike riding
Men put a lot of pressure on their genitals when riding a bike. Compressing the perineum (the area between the scrotum and anus) on a bicycle seat can stop blood flow to this area, causing sexual difficulties. Men are advised to use a noseless bicycle seat, adjust their position on the bicycle so that there is less pressure on the perineum, and limit the time they spent bike riding.